Download full member briefing as PDF Download full submission as PDF
Key messages
A COTA Victoria survey has found that many older women experiencing chronic pain struggle to find effective support and feel marginalised by health services that lack necessary empathy and understanding. Too often, women feel that they are expected to just be stoic and accept pain as an inevitable part of ageing.
While some women reported positive experiences with local health providers, the overwhelming majority found no or limited pain management benefit from services. Systemic problems include long waiting lists, prohibitive costs and barriers to medication.
Feedback suggests that most older women with chronic pain want better help from medical and allied health practitioners in local, in-person settings. There is also scope for improving help through online, peer and social and activity-based programs.
The survey
Between February and March 2024, COTA Victoria conducted an online survey of older women through our membership network and associated social media channels. A total of 75 women responded, 55% of which were aged 65-79, 14% aged 80 and over, and 31% aged 50-64.
While not a representative sample, this data provides a valuable insight into pain related experiences of older women across Victoria and their suggestions for improved responses.
The survey was conducted in the context of the current Victorian Government Inquiry into Women’s Pain. The findings informed COTA Victoria’s submission to the inquiry, which can be found on the COTA Victoria website.
We asked women to share experiences of seeking help for chronic pain, how effective the help was and what aspects they found positive or negative. We also asked them to rate their likelihood of approaching a range of different services and supports. Finally, we asked women to comment on the pain issues that needed most attention in the Victorian health system.
“I just take a Panadol or six on days I can’t cope and cry. I’ve fallen through a very large crack.” – COTA Victoria survey respondent
Summary of findings
- The main pain related conditions women nominated included endometriosis, cancer, spinal, back, and hip problems, fibromyalgia, migraine and – most common of all – arthritis.
- In almost half of cases, help for chronic pain was sought before any diagnosis, with pain being the primary concern. A further 16% were unsure whether their pain was associated with a pre-diagnosed medical condition.
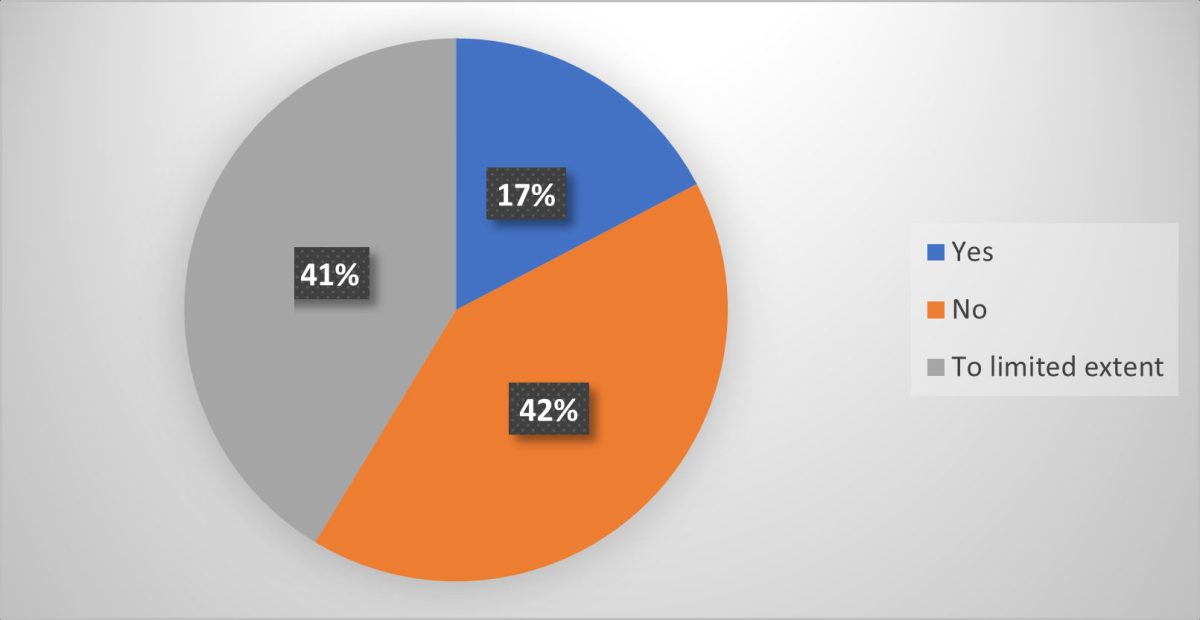
- Respondents reported very mixed effectiveness of the help they accessed. Overall, 40% said the help was not effective and a further 43% described it as having only limited benefit (see Figure 2).
- Help-seeking experiences were often dominated by concerns about a lack of knowledge about where to turn to access help and GP disinterest, dismissal, and minimisation of their problems.
- Lack of empathy from doctors and a feeling of not being listened to due to age and gender was a strong theme in many responses. Some were told that pain was “part of getting old” and that they needed to “just get used to it”.
- Positive experiences, while less often cited, included good advice and referral from trusted GPs, and helpful treatment by allied health practitioners (although this was often seen as too costly to maintain).
- Systemic issues raised included prohibitively long waiting lists for specialist pain clinics, with many being told to not even bother trying to access these services. Waiting times for surgery were also raised, with some saying they lacked effective pain management during this time.
- Access to medication was a common concern, while others expressed concern at over-reliance on drug prescription. Responses included frustration at the difficulty in accessing drugs they found helpful, such as resentment at being treated as potential addicts while not being offered feasible alternatives.
Preferred sources of help
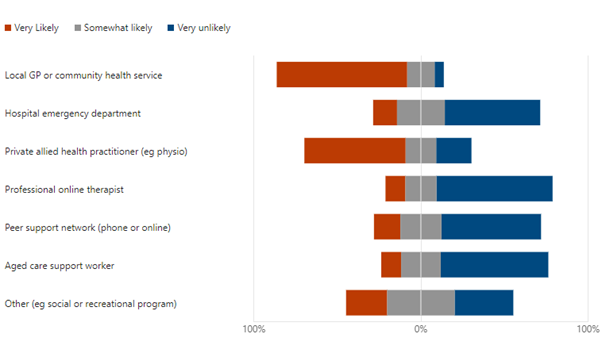
Feedback on where older women would be likely to seek help varied quite widely but with some clear patterns (see Figure 2). The key takeaway points included that:
- The most consistently likely destination was local GPs and community health services (78% very likely), with only 15% being very likely to visit a hospital emergency department for pain support.
- Allied health practitioners received a positive response with over three quarters of respondents somewhat or very likely to use them. Yet nearly a quarter of respondents reported being very unlikely to use them (possibly – on the basis of answers to previous questions – due to cost, accessibility and lack of good referral systems).
- A majority of respondents were unlikely to use an online professional therapist, with only 12% being very likely and 75% very unlikely to do so.
- Peer support in any form was seen as an option by less than half, with nearly 60% saying they were very unlikely to seek such support.
Suggested solutions
Ideas put forward by respondents on how the system could be improved for older women seeking pain management support included:
- better availability of pain management options – including availability of a professionally developed pain management plan reviewed every 6-12 months, local community-based pain management support groups and tailored physical activity programs, and more pain related support to be provided through the aged care system.
- better access to relevant community-based healthcare – including dedicated women’s health clinics with interest and expertise in older women’s issues, more effective referral by GPs to allied health practitioners and lower cost options to allow for more sustained allied health care.
- better access to appropriate specialist care – including reduced waiting times for specialist pain clinics and access to specialist aged health practitioners within universal health services, increased training opportunities for doctors on older women’s conditions and especially on empathetic communication.
- increased research on key older women’s pain issues, such as post-menopausal pain, designed to inform effective care.
The feedback and contributions from the survey informed COTA Victoria’s submission to the Inquiry into Women’s Pain, including our recommendations for the Inquiry, which are informed by the suggestions that survey respondents provided.
How can you stay engaged on these issues?
The Victorian Government’s Inquiry into Women’s Pain is open for input until 31 July 2024. Online surveys for women and girls, for carers and for clinicians can be accessed through the Engage Victoria website. This website also includes an option to register to stay engaged with the Inquiry as it progresses.
COTA Victoria will continue to promote issues relating to older women and chronic pain as part of our broader priority focus on better health and health care experiences for all older Victorians. This work includes activities involving volunteer peer advisors sharing their professional and personal experiences.
Seeking more information?
If policy, research, or academic organisations are interested in further understanding our survey and findings, please contact Martin Turnbull, our Senior Policy Advisor.
As we continue to engage on issues related to ageing and health, we are keen to hear from members on their experience of the health system. Similarly, for input related to health policy, contact Martin Turnbull, our Senior Policy Advisor.
Please also feel free to contact us on matters directly affecting you by emailing askcota@cotavic.org.au or calling us on 1300 135 090.
